PREGNANCY
This is the first of a series of two articles regarding musculoskeletal clinical issues and phycological change in the women body during and after pregnancy and how exercises can help to reduces the symptom of these ones.
The aim of this article is to answer questions that some women may have and help them to find solution to some recurrent pregnancy problem through exercises. In any case, if you are pregnant, GO SEE your doctor BEFORE engaging any kind of physical activity. I’m not a doctor and this article only relate the most relevant finding regarding pregnancy and the effect of physical activity during and after the gestational period.
Pelvic girdle pain and low back pain
Pelvic girdle pain (PGP) is pain experienced between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the sacroiliac joints. The prevalence rate of pregnancy-related LBP and PGP is estimated to be about 50% during pregnancy.
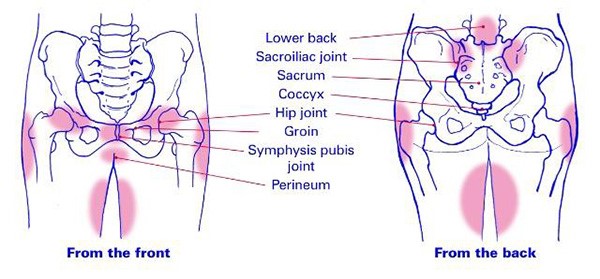
Figure 1 : CARTWRIGHT, J. (2019, August 29)3
The causes of Pelvic girdle pain are uncertain and probably multifactorial. The pelvis transfers load from the trunk to the legs and this requires a stable pelvis. Overload of the ligaments of the pelvis may be a result of impaired load transfer during activities and hence have an influence on PGP. The sacrospinous and the long dorsal sacroiliac ligament are both thought to be a possible source of pain in PGP. The changes in spinal curvature during pregnancy as well as frequent or sustained pain-provoking postures might influence the pelvic ligaments, causing pain1.
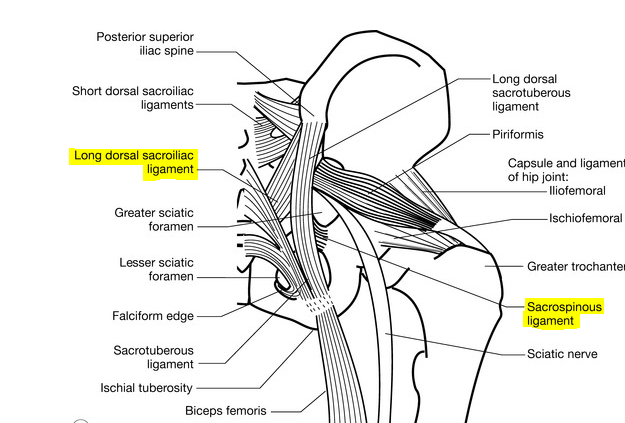
Figure 2 4
According to the European guideline for PGP, individualized exercises to treat PGP in pregnancy are recommended. 1
Moreover, there is few evidence that exercises can prevent Pelvic girdle pain and low back pain. Further, women who reported high-impact exercise 3–5 times per week before pregnancy, like running or jumping, had a 14% lower risk of developing severe PGP in pregnancy compared with non-exercisers. 1
Pelvic floor dysfunction
Pelvic floor dysfunction (PFD) is defined as the presence of symptoms as a complaint of involuntary passing of urine, involuntary passing of faeces or flatus or pelvic organ prolapses. The conditions can present separately or coexist. 1
Involuntary passing of urine and / or faeces or flatus are cause by either stress; the complaint of involuntary leakage on effort or exertion (eg, sporting activities), or by sneezing or coughing. They can be cause also by a sentiment of urgency.1
Pelvic organ prolapse (POP) is ‘the descent of one or more of the anterior vaginal walls, posterior vaginal wall, the uterus (cervix), or the apex of the vagina (vaginal vault or cuff scar after hysterectomy)’. The presence of any such sign should be correlated with relevant POP symptoms. POP ranges from asymptomatic minor changes in vaginal support, common after childbirth, to severe vaginal bulging for which women choose treatment. 1
Risk factors for PFDs include pregnancy and childbirth-related factors (injuries to peripheral nerves, connective tissue and muscles), heritage and ethnicity, obesity, behavioural factors,
ageing, and strenuous work. Vaginal birth is the strongest risk factor for POP in women of all ages, while vaginal birth increases the risk for involuntary passing of urine by about two-fold in younger and middle-aged women, but no longer plays a role in older women. 1
According to the most recent Cochrane review, in the general population, pregnant women without randomly assigned to intensive antenatal pelvic floor muscle training were less likely to report involuntary passing of urine and faeces or flatus up to 6 months after delivery. 1
Diastasis recti abdominis
Diastasis recti abdominis (DRA) is an impairment with midlinen separation of the two rectus abdominis muscles along the linean alba. 1 Prevalence rates (with and without protrusion/hernia) during pregnancy vary between 27% and 100% in the second and third trimester. 1 There is no evidence in the current literature that exercises or training abdominal can prevent or help with the diastasis of recti abdominis.
Exercises Recommendation
Through this article, they were few evidences that exercises could prevent or diminish symptoms of pelvic gridle pain, lower back pain and the diastasis of the recti abdominis. Moreover, pelvic floor strengthening seems to be the best way to prevent pelvic floor dysfunction during and after pregnancy. Will be presented in the following pages sevens exercises to strengthen this region.
Through this article, they were few evidences that exercises could prevent or diminish symptoms of pelvic gridle pain, lower back pain and the diastasis of the recti abdominis. Moreover, pelvic floor strengthening seems to be the best way to prevent pelvic floor dysfunction during and after pregnancy. Will be presented in the following pages sevens exercises to strengthen this region.
Activation of the pelvic floor 2
Starting position: Lie on your back, find your pelvic floor muscles. To do this, contract the muscle between your vagina and your anus by pulling its center inward. Avoid contracting your glutes while contracting your pelvic floor. Be careful to not contract the urinary and / or anal sphincters muscle instead.
Step 1 : Breathe in and contract your pelvic floor
Step 2: Breathe out and relax the muscles
Repeat for ten to twenty breath
Activation of the transverse abdominis and the pelvic floor 2
Lie on your back and contract simultaneously your transverse abdominis and your pelvic floor muscles. Repeat the same protocol as seen in the two previous exercises
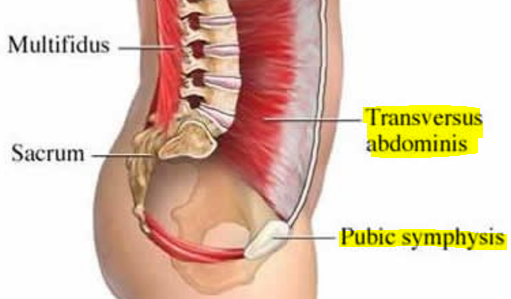
Figure 3 : Gordon & Reed,. (2018) 5
Half-bridge 2
Ascent: Lie on your back, knee bent at 90o and feet to the width of your hips. Breathe out, lift your hips up. Breathe in and keep the position. Contract your transverse abdominis
Descent: Breathe out and unfold one vertebra at the time on the ground from the head to the hips. Breath in, relax your transverse abdominis and repeat for ten to twenty breath.
Table 2
Starting position: In quadruped position, knees under the hips, hands under the shoulders and a straight back
Step 1 : Breathe out, extend the right leg until it is horizontal. Simultaneously, extend the left arm until it is horizontal, with your thumb pointing the ceiling.
Step 2 : Breathe in and come back to the starting position. Repeat on each side for ten to twenty breath.
Tips : if too difficult, raise only one limb at the time. You shouldn’t rotate or twist while your elevating your limbs
Plank 2
Starting position: Facing the ground, resting on the elbows slightly apart and put your feet together.
Step 1 : Engage the transverse abdominis and the pelvic floor. Image to Pull your shoulder blades towards your back pockets.
Step 2 : Push on your elbow and your feet to get of the ground Squeeze your glutes and maintain that position from 5 to 30 breath.
Tips: Be careful to always have a straight back. Your hips should be at the same level as your shoulders
Pelvic equilibration 2
Starting position: Lie on the back. Your knees should be bent and legs and feet hip-width apart, with a cousin or ball between the knees. Arms along the body, palms against the ground
Step 1 : Breathe out, push your knee together, engage the transverse abdominis and the pelvic floor and lift your hips off the ground. Be careful to put the same amount of pressure under each foot. Breathe in and maintain the position.
Step 2 : Breathe out, unfold one vertebra at the time on the ground from the head to the hips Keep pushing your knee together and engaging the transverse abdominis and the pelvic floor. Once your back again the floor, breathe in and relax your knees, the transverse abdominis and the pelvic floor muscles. Repeat for 10 breath
Tips : Be careful to keep your knees align with your hips.
Reference :
- Bø K, et al. Br J Sports Med 2016;50:571–589. doi:10.1136/bjsports-2016-096218
- Harvey JF,2011, Chapitre 6 : Les exercices, Paré E (Ed), L’entraînement spinal : 80 exercises pour en finir avec les maux de dos (pp113-115,178,181,184,193), Montréal, Québec, Les éditions de l’homme
- CARTWRIGHT, J. (2019, August 29). 5 Life Hacks to Help Relieve Pelvic Girdle Pain (PGP). Retrieved December 2, 2020, from https://sportandspinalphysio.com.au/5-life-hacks-to-help-relieve-pelvic-girdle-pain-pgp/
- Unknown, (2016, September 11). Common presentations and diagnostic techniques. Retrieved February 14, 2020, from https://musculoskeletalkey.com/common-presentations-and-diagnostic-techniques/#f0190
- Emerich Gordon, K., & Reed, O. (2018). The Role of the Pelvic Floor in Respiration: A Multidisciplinary Literature Review. Journal of Voice. https://doi.org/10.1016/j.jvoice.2018.09.024
Related articles :
Benjamin DR, van de Water AT, Peiris CL. Effects of exercise on diastasis of the rectus abdominis muscle in the antenatal and postnatal periods: a systematic review. Physiotherapy 2014;100:1–8.
Boyle R, Hay-Smith EJ, Cody JD, et al. Pelvic floor muscle training for prevention and treatment of urinary and faecal incontinence in antenatal and postnatal women. Cochrane Database Syst Rev 2012;(10):CD007471.
Bump RC, Norton PA. Epidemiology and natural history of pelvic floor dysfunction. Obstet Gynecol Clin North Am 1998;25:723–46.
Haakstad LA, Bo K. Effect of a regular exercise programme on pelvic girdle and low back pain in previously inactive pregnant women: a randomized controlled trial. J Rehabil Med 2015;47:229–34.
Haakstad L, Telenius E, Bø K. Exercise and pelvic girdle pain during pregnancy. Are there any associations? Open J Obstet Gynecol 2013;3:520–7.
Kari Bø, Marie Ellstrøm Engh, Gunvor Hilde, Regular Exercisers Have Stronger Pelvic Floor Muscles than Non-Regular Exercisers at Midpregnancy, American Journal of Obstetrics and Gynecology, , DOI: 10.1016/j.ajog.2017.12.220
Ostgaard HC, Zetherstrom G, Roos-Hansson E, et al. Reduction of back and posterior pelvic pain in pregnancy. Spine 1994;19:894–900
Owe KM, Bjelland EK, Stuge B, et al. Exercise level before pregnancy and engaging in high-impact sports reduce the risk of pelvic girdle pain: a population-based cohort study of 39 184 women. Br J Sports Med Published Online First: 4 October 2015 doi:10.1136/bjsports-2015-094921
Ostgaard HC, Zetherstrom G, Roos-Hansson E, et al. Reduction of back and posterior pelvic pain in pregnancy. Spine 1994;19:894–900
Stafne SN, Salvesen KA, Romundstad PR, et al. Does regular exercise during pregnancy influence lumbopelvic pain? A randomized controlled trial. Acta Obstet Gynecol Scand 2012;91:552–9.
Vleeming A, Albert HB, Ostgaard HC, et al. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J 2008;17:794–819.